Insights
A value-based healthcare approach to significantly reducing the health impacts and costs of interpersonal violence
Interpersonal violence represents a public health challenge in the US with profound negative public health and economic impacts. Programmatic interventions oriented toward addressing the downstream costs associated with violence are generally unavailable to victims of violence within traditional healthcare settings. To address both the acute and ongoing impact of interpersonal violence while reducing the total cost of care for violence victim populations, a program must deliver evidence-based interventions that are data driven, scalable, tech-enabled, and capable of keeping vulnerable populations longitudinally engaged. Sustained engagement is key to meaningful, long-term behavior change and should be personalized to address individuals’ everyday safety and support needs. To succeed, these programs must connect with people from a wide range of backgrounds and life experiences—and do so in a way that earns and keeps their trust. Making these programs economically sustainable by generating a positive return on investment (ROI) is key to increasing their impact on health and expanding a strong network of coordinated support services for vulnerable populations across the U.S, particularly for US health plans that bear full total cost of care risk.
As a trusted in-network provider for US health plans, Mindoula offers a violence reduction program that embodies all the characteristics listed above, and that functions as an extension of payor capability sets in serving complex and specialty populations. Named the Mindoula Interpersonal Violence Reduction Program (IVRP), Mindoula’s interpersonal violence reduction program is a data-driven, integrated care extension approach to interpersonal violence reduction that is available across the US, is currently active in 7 US states, and has been affirmatively proven effective in reducing violence-related healthcare utilization and costs. In multiple payor-validated, pre/post analyses utilizing precision matched controls for cost comparison during the relevant program period, the IVRP has demonstrated a reduction in emergency department visits, hospital admissions, and overall healthcare costs. It has done so by leveraging predictive analytics to identify at-risk individuals, proactively engaging them with personalized support, and integrating targeted interventions that address behavioral, medical, and social determinants of health. Total cost of care savings have been calculated and approved by the payors’ value-based care data science teams, through which value-based bonuses were paid to Mindoula in connection with payor-validated total cost of care reductions in the populations served. Across multiple Medicaid markets, the IVRP has delivered a 2.8x to 4.3x return on investment while improving health outcomes. In so doing, the IVRP has also meaningfully reduced health disparities, and improved health equity in the populations served.
These results demonstrate that it is possible to adopt and implement scalable, technology-enabled programmatic solutions that mitigate the impact of interpersonal violence while improving the health of vulnerable populations in an economically sustainable way. The goal of this paper is to advance and inform the dialogue around improving health equity and reducing health disparities related to interpersonal violence. The evidence presented in this paper aims to encourage efforts across the US to do more than we are doing collectively today to support and care for victims of interpersonal violence, specifically to advocate for expansion of payor-led violence reduction efforts that directly benefit those individuals and families programmatically served, while also delivering many indirect benefits to the nation at large, and society as a whole.
Understanding the Challenge of Interpersonal Violence
Interpersonal violence (IPV) is a highly prevalent and costly public health problem in the United States. IPV involves the intentional use of force or power against others, leading to harm, and even death. It may be physical, sexual, or psychological, and may fall into well-known categories such as interpersonal violence, intimate or intimate partner violence, community-based violence, Adverse Childhood Experiences (ACE), youth violence, workplace violence, and bullying, among other categories. Regardless of its form or category, IPV causes long-lasting, negative effects on mental and physical health and well-being, creating a heavy burden on both individuals and society as a whole (Blasdell 2021). According to the CDC, approximately 2 in 5 women and 1 in 10 men report experiencing sexual or physical interpersonal violence in their lifetime. Additionally, almost half of all US men and women report at least one form of psychological victimization (Basile 2022). Psychological, physical, and sexual IPV often lead to long-lasting mental health conditions such as depression, post-traumatic stress disorder, anxiety, substance use, and low self-esteem (Blasdell 2021). Adverse childhood experiences are associated with increased risk of chronic medical conditions, while intimate partner violence specifically has been linked to risk for diabetes, heart disease, thyroid disorders, and cancer (Weitzman 2020, Thurston 2022). The annual economic impact of IPV ranges from a CDC estimate of $8.2 billion to approximately $196.1 billion (or 3% of the US Gross Domestic Product reported by the World Bank in 2017) (Mercy 2017).
The extensive nature and the negative individual and societal impacts of IPV have led to the development of a diverse range of prevention programs across the US healthcare system, education system, and various other state public health entities. However, these programs all fall short in important ways. In the healthcare system, hospitals and care providers offer hospital-based violence intervention (HBVI) programs to combat violent injury in communities which impact millions of Americans annually. Although HBVI programs connect victims of community-based violence to community support following hospital discharge, these programs focus primarily on firearm-related violence, leaving other forms of interpersonal violence, such as intimate partner violence, largely unaddressed (Webster 2022). Additionally, healthcare providers often lack the resources, incentives, and training necessary to carry out post-screening measures, resulting in missed opportunities to provide meaningful support and treatment after the clinical visit that included the violence screening (Trabold 2020). In the US education system, school-based strategies, cognitive-behavioral therapy, parental training, and peer mediation emphasize the importance of targeting individual, relational, and community factors in addressing the problem of violence (Fazal 2024). Finally, in the public sector more broadly, IPV prevention at the state level is generally administered by various state agencies, including state health departments and social service organizations, and focuses on screening, training healthcare providers, and promoting trauma-informed practices. While such trauma-informed practices often recommend follow-up steps to address co-occurring mental health and substance use disorders, along with interventions that promote problem-solving, decision-making, and healthier self-perception, public sector efforts typically focus upon screening for violence exposure rather than the delivery of robust, integrated violence prevention interventions.
A survey of existing clinical and research studies as well as other literature in the violence risk reduction and prevention space highlights important shortcomings in solutioning. Multiple research studies focused on interpersonal violence highlight a significant gap between the screening for violence risk on the one hand, and the implementation of effective follow-up violence prevention and the violence reduction interventions necessary to address the problem on the other hand. A large body of research brings attention to the fact that IPV screening programs delivered across a range of settings often have limited violence reduction success due to insufficient follow-up care. Finally, despite nearly universal acknowledgement in the literature that the analysis and tracking of the cost-effectiveness of violence and prevention and intervention efforts is critical to justify additional investment in these programs, recent data on cost effectiveness for violence prevention programs is limited (Sheppard 2024, O’Toole 2024).
Health plans and other organizations hold full population health risk for the total cost of care associated with treating the immediate effects of violence related injuries, but they are also financially responsible for the more intractable downstream impacts of violence upon mental and physical health which often includes avoidable health costs. Therefore, established, proven interpersonal violence prevention and reduction programs such as the IVRP that identify risk and then address that risk in a scalable and effective way, while rigorously tracking and analyzing the cost effectiveness and return on investment of such programs, offer a compelling opportunity for health plans interested in reducing the cost burden associated with insuring populations impacted by interpersonal violence. This is especially true when a partner is willing to contract for such a program under a value-based economic model in which service fees can be put at risk in return for a gain share arrangement calculated with reference to total cost of care reductions net of program fees.
Mindoula’s Approach: A Data Driven, Cost Effective Interpersonal Violence Reduction Program For Payors
Mindoula’s Interpersonal Violence Reduction Program (IVRP) is a 24/7, team-based, technology-enabled virtual and in-person care extension solution for US health plans that complements, and extends from, each payor’s unique internal care and support capabilities. The IVRP identifies, engages, and serves adult victims of interpersonal violence, including perpetrators of violence who are, or have been, victims of violence themselves. The IVRP includes coordinated supportive services for health plan members who have experienced acts of intimate partner, family, and/or community-based violence. The program consists of a highly individualized series of violence-related and safety-related, social determinants of health-focused, cost-reducing interventions delivered virtually and in person by teams of community health workers, peer support specialists, clinicians, and case managers trained in the delivery of the IVRP model. The IVRP model includes interventions that enhance member skills and reduce the occurrences of potentially violent situations. IVRP elements include care coordination, health system navigation support, psychosocial education, skills training, as well as micro and macro therapies designed to empower IVRP program members to make the behavior and life changes necessary to break the cycle of violence that has negatively impacted their health and wellbeing.
To identify individuals who may be at risk for violence exposure and who will benefit from becoming a member of the IVRP, Mindoula securely ingests into its HIPPA compliant HITRUST certified Mindoula Member Registry platform (mMR) historical payor claims in order to analyze more than 40,000 violence-related claim types, divided into what Mindoula labels “Level 1” and “Level 2” violence claims. Level 1 violence claims typically include diagnoses of violence indicating abuse, trauma/injury, and/or physical harm, whereas Level 2 claims generally suggest the potential of violence (e.g. injury to head and neck, intentional self-harm) and are subsequently validated during member screening and intake. Mindoula stratifies member cohorts by violence type algorithmically, using a taxonomy of diagnostic codes and code sets that match member violence risk profiles with payor utilization data such as emergency room visits, hospitalizations, pharmacy spend, and annualized cost of care. This stratification process utilizes member archetypes that Mindoula’s adaptive analytics process continuously derives and refines to inform member selection and outreach. Based upon this member stratification and identification process, Mindoula’s mMR platform generates a prioritized member outreach list of those members most likely to benefit from enrollment in the IVRP.
Individuals identified through risk stratification are eligible for enrollment in the IVRP if they are an active health plan member aged 18 or older with one or more violence-related diagnoses in the previous 24 months, who are not enrolled in an exclusionary health plan program, and whose total cost of care and utilization patterns meet pre-defined thresholds. The IVRP outreach team uses telephonic, text, and feet-on-the-street outreach to engage eligible members and enroll them in the program. Mindoula’s team of clinical and non-clinical care extenders have diverse backgrounds, areas of concentration, education levels (at least bachelor’s-level with relevant certification up to master’s level licensed clinicians), and personal experiences that enable them to serve members with a range of personal needs and experiences. In addition, all care extenders have specialized training and experience interacting with individuals exposed to intimate partner and community violence. Each enrolled member receives virtual and in-person support with 24/7 coverage specifically tailored to that member’s violence-related circumstances, and personalized to meet their day-to-day safety and support needs. Using proprietary psychometrics and predictive analytics, the Mindoula Messenger secure texting app, and multi-platform engagement tools, IVRP care extenders stay engaged with member populations across a range of varied demographics and unique person circumstances during a service period that is typically 6 to 12 months in duration. During this period of sustained engagement, Mindoula’s care extenders help members address behavioral health, physical health, and social determinants of health (SDoH) needs in tandem with the delivery of violence-related supports and services. The IVRP also includes specialized content and support for newly pregnant and postpartum mothers, and has even proven effective with prenatal and postpartum mothers addicted to opioids and other addictive substances.
Core aspects of the IVRP program orient toward addressing unmet physical, behavioral, and social determinants of health needs while evaluating safety and engaging in ongoing safety planning. Embedded program interventions focus on building empowerment, education on cycles of violence, and providing support to establish healthy boundaries. A measurement-based approach is a core program feature utilizing both evidence-based assessment and standardized program-specific tools to capture initial symptoms and needs, monitor interim progress, and evaluate post-program efficacy. Supportive interventions are designed to build capacity for independence through collaborative recruitment of financial, educational, employment, and housing supports. Engagement of the family system includes resource development for any impacted minors in the household, ensuring connection with available community and health plan resources, and facilitating community referrals to address more severe psychological and medical impacts of violence.
There is a range of interpersonal violence that can be successfully addressed under the IVRP, ranging from non-physical to physical, one-time or sustained, involving weapons or not involving weapons. Regardless of the type, severity, or duration of interpersonal violence, the ability to ameliorate the harm associated with interpersonal violence aligns with US health plans’ mission to foster healthy communities.
In delivering the IVRP as a partner to US health plans, Mindoula contracts with the health plans at two levels within the health plan organization. At the corporate level, Mindoula executes an agreement that enables data sharing and member outreach, and then at the state level, Mindoula signs a provider agreement with the state-based Managed Care Organization (MCO). The provider agreement includes a state-specific Statement of Work (SOW) that includes standard pricing and terms of service delivery for health plans members enrolled in the IVRP. At the election of the MCO, the SOW includes value-based elements under which Mindoula places at risk its provider fees in return for a gain share percentage of total cost of care savings generated by the IVRP net of fees, under an industry-endorsed and validated propensity matched pre/post analysis using a matched control.
Program Participant Characteristics
VRP supports a complex population with a high burden of comorbid social, medical, and behavioral health needs. To date, Mindoula has served over 15,000 individuals across seven (7)
- Average age: 44-years-old
- 72% female
- 90% reported exposure to family or community violence
- 87% having a behavioral health diagnosis upon enrollment
- Average of 6 chronic medical conditions per member
- Average of 5 chronic behavioral health conditions per member
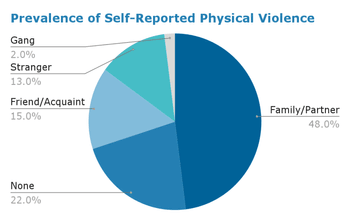
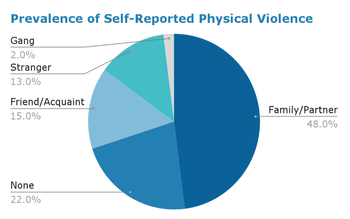
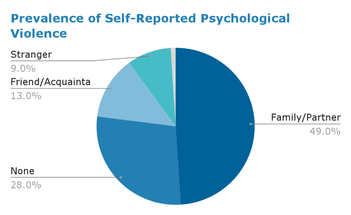
states. In the year 2023, 4,622 individuals were actively served for 60 days or longer and are subsequently characterized in this issue brief. The average age was 44 and the majority were female (n=3,316, 72%). The IVRP intake process includes detailed trauma and violence exposure screening to inform measurement-based care. Nearly 90% had witnessed family or community violence, and consistent with published literature, physical and psychological violence were the most commonly reported types of violence experienced (Figure 1). When present, experiences of violence were most often perpetrated by family members or a partner (Figure 2).
Figure 1. Prevalence of Self Reported Violence
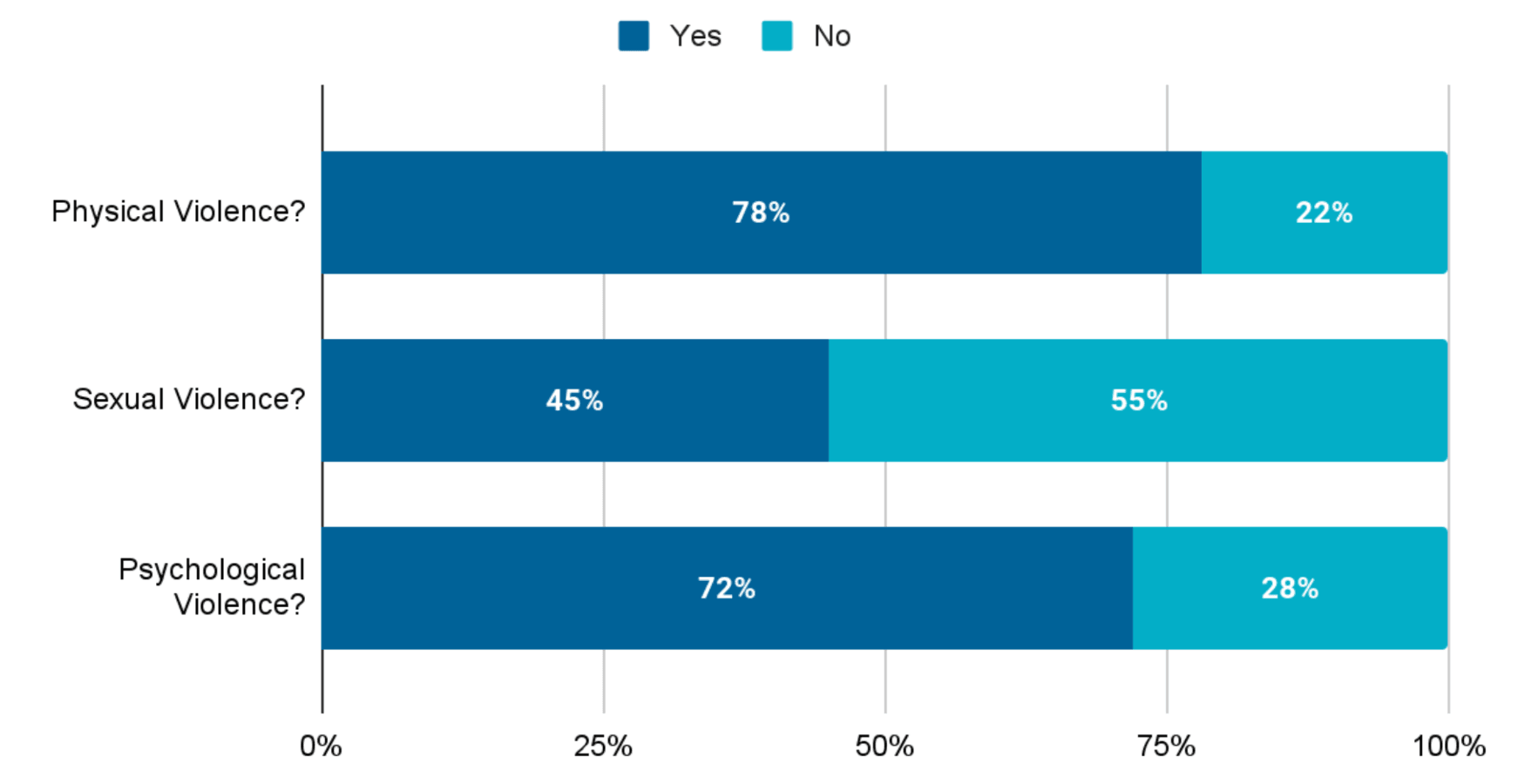
Figure 2. Self-Reported Interpersonal Violence Perpetrator Types
Upon enrollment, 87% had a behavioral health diagnosis with an average of 5 chronic behavioral health conditions per person identified by claims. Based on the multi-diagnostic My Mood Monitor Checklist (M3) (Gaynes 2010) completed at intake, 52% of members indicated at least one unmet behavioral health need not previously identified in claims. Finally, this population also represented significant medical co-morbidity, with an average of 6 chronic medical conditions per person reported in claims. The top 10 medical and behavioral health conditions are depicted in Table 1.
| Table 1: Most Prevalent Medical and Behavioral Health Conditions | |
|---|---|
| Chronic Condition | % Mindoula Members |
| Anxiety Disorders | 69.8% |
| Depression Disorders | 63.8% |
| Hypertension | 55.3% |
| Fibromyalgia, Chronic Pain, & Fatigue | 50.8% |
| Obesity | 49.7% |
| Tobacco Use | 49.0% |
| Hyperlipidemia | 46.0% |
| Drug/Alcohol/Opioid Disorders | 42.4% |
| Rheumatoid Arthritis/Osteoarthritis | 41.0% |
| Anemia | 34.1% |
The Health Related Social Needs (HRSN) assessment identifies non-medical factors that impact health outcomes, including food insecurity, housing instability, transportation barriers, utility difficulties, interpersonal violence, and other social determinants that can significantly affect a person's ability to maintain good health and access healthcare services. (Billioux 2017). A total of 94% (n= 4,355) completed the HRSN in which they reported an average of 8 unmet social needs. In addition, 84% (n=3,658) of these respondents reported experiencing stress or anxiety in their daily lives (Figure 3).

Program Outcomes: Meaningful Impact at Scale
The return on investment analyzed for 2,754 program participants across three deidentified state-wide Medicaid markets (n=1,746; 718; 290), is representative of Mindoula’s overall service population. As seen in Table 2, all markets experienced a positive ROI ranging from 2.8 to 4.3 times investment NET of program fees, and Market 1 (n=1,764) had adequate volume to support a subgroup ROI analysis (Table 3). In Market 1, 65% of the cohort were female (n=1,141), with an average age of 44, and 8 unmet social needs identified on average at intake. Similar to our cross-market population, 89% of this cohort had behavioral health needs (n=1,576) and 95% had one or more chronic medical conditions (n=1,674).
The Mindoula Precision Matched Control ROI analysis methodology employs advanced propensity score techniques and high-dimensional matching algorithms to conduct rigorous savings analyses. The approach implements a 1:1 nearest neighbor precision matching protocol, validated through placebo testing, to identify optimal control cohorts for program participants. The methodology is specifically calibrated for complex populations with severe conditions and high-cost utilization patterns.
The analytical framework incorporates longitudinal data spanning customized evaluation windows: a robust baseline period (12-24 months pre-intervention) and a subsequent intervention period. The matching algorithm synthesizes multiple dimensional parameters including demographic characteristics (e.g., age, gender), utilization patterns (measured as days served, representing the annualized number of days on which members received services related to confirmed violence), clinical risk predictions (e.g., rising risk predictive modeling), and comprehensive disease burden profiles encompassing 30 standardized chronic conditions from the Chronic Condition Warehouse, with particular emphasis on mental health and potentially disabling conditions (Centers for Medicare & Medicaid Services, 2022). To ensure methodological validity and statistical robustness, the analysis incorporates multiple sensitivity analyses, including systematic outlier detection and validation through extended baseline period analyses.
Return on Investment (ROI) Analysis Across Medicaid Markets:
Analysis of program impact across three markets demonstrated significant cost savings and positive return on investment (ROI) (Table 3). Market 3 was predominantly female (95%) while Markets 1 and 2 served one-third males.
ROI Analysis Across Medicaid Markets:
- Utilization Reductions: Reduction in Emergency Department (ED) visits and hospitalizations by over 50%.
- Net ROI: Ranging from 2.8x to 4.3x.
- Cost Savings: Up to $12,681 PMPY in Market 2.
- Confirmed Violence-Related Costs: Decreased by 15%-47%, highlighting reduced utilization of acute care services.
Chronic condition prevalence was balanced between Mindoula and controls. Across markets, anxiety disorders were most prevalent (52%-72%), followed by depression (45%-65%), and hypertension (33%-61%). Market 1 represented a population with higher clinical complexity and resource utilization, as evidenced by both chronic conditions and baseline costs ($42,056 PMPY), which were more than double those of Market 3 ($20,329 PMPY) and significantly higher than Market 2 ($29,394 PMPY). Similarly, confirmed violence-related costs in Market 1 were the highest ($821 PMPY), exceeding Market 2 ($419 PMPY) and Market 3 ($559 PMPY), indicating a population with significant exposure to violence-related healthcare utilization.
The IVRP program demonstrated strong financial sustainability through consistent positive return multiples across all markets. Market 2 achieved the highest return multiple at 4.3x ($12,681 PMPY), while Markets 1 and 3 both realized 2.8x returns on investment ($8,349 PMPY and $8,372 PMPY Total Cost of Care savings, respectively). These results indicate that the IVRP program was successful in reducing healthcare costs across all measured categories, with particularly strong performance in Market 2. The consistent positive return multiples suggest that the intervention is financially sustainable while delivering meaningful reductions in confirmed violence-related healthcare utilization, even in populations with complex clinical needs and high baseline costs.
Despite having the lowest pre-intervention total cost of care ($20,329 PMPY), Market 3 showed disproportionately high confirmed violence-related costs ($559 PMPY) and emergency department utilization ($2,349 PMPY) in the pre-intervention period relative to its overall spending. This market achieved the most dramatic improvements in these areas, with a 45% reduction in confirmed violence-related annual service days, substantial pharmacy savings of 98% (driven by a 25% decrease in Mindoula group vs 55% increase in Control group), and post-intervention total cost of care savings of $8,372 PMPY, suggesting the intervention was particularly effective in addressing acute care needs and medication management for this population. Markets 2 and 3 achieved reductions in total cost of care of $12,681 PMPY and $8,349 PMPY as well as reductions in violence-related costs of 15% ($125 PMPY) and 47% ($200 PMPY), respectively. The relative reduction for Market 1 was lower, reflecting the higher clinical complexity of this population while still demonstrating the care model's effectiveness in improving outcomes for highly complex patients.
Acute care utilization patterns varied across markets in the pre-intervention period. Market 3 showed the highest relative emergency department costs ($2,349 PMPY) compared to Markets 1 and 2 ($1,328 and $746 PMPY, respectively). However, inpatient admission costs were relatively consistent across markets, ranging from $6,764 to $8,834 PMPY. The intervention demonstrated strong effectiveness in reducing both admission and emergency department utilization across all markets. Particularly notable was Market 2's 78% savings in inpatient admission costs compared to controls at $5,284 PMPY. Alongside savings for emergency department visits (without admissions), these data demonstrate the program's success in reducing emergency department visits and associated inpatient admissions through improved care management and prevention strategies.
In addition to evaluating the overall ROI, subgroups within the largest market with significant cost benefit were identified (Table 4). These results show highest ROI for those with substance use and sustained positive ROI for common medical conditions such as diabetes and heart disease. A substantial group of 886 members with fibromyalgia, chronic pain, and fatigue achieved a 3.0x return multiple, suggesting the program's effectiveness extends to populations with chronic pain conditions.
| Table 2: Return on Investment 2023 Market Comparison | ||||||
|---|---|---|---|---|---|---|
| Market 1 | Market 2 | Market 3 | ||||
| Mindoula | Matched Control | Mindoula | Matched Control | Mindoula | Matched Control | |
| Members Served | 2,110 | 1,046 | 367 | |||
| Members Evaluated | 1,746 | 1,746 | 718 | 718 | 290 | 290 |
| % Male/Female | 35%/65% | 35%/65% | 33%/67% | 33%/67% | 5%/95% | 5%/95% |
| Age (Average) | 44 | 45 | 43 | 43 | 35 | 35 |
| Chronic Conditions | ||||||
| Hypertension | 59% | 61% | 53% | 52% | 33% | 30% |
| Anxiety Disorders | 72% | 70% | 66% | 67% | 52% | 53% |
| Depression | 57% | 58% | 63% | 65% | 45% | 45% |
| Fibromyalgia, Chronic Pain and Fatigue | 51% | 46% | 48% | 43% | 34% | 33% |
| Obesity | 51% | 46% | 46% | 40% | 33% | 35% |
| Pre-Period | ||||||
| Total Cost of Care PMPY | $42,056 | $42,045 | $29,394 | $28,711 | $20,329 | $20,026 |
| Pharmacy Cost PMPY | $24,275 | $24,047 | $16,063 | $14,380 | $3,569 | $4,774 |
| Medical Cost PMPY | $17,782 | $17,998 | $13,331 | $14,331 | $16,760 | $15,251 |
| Admissions Cost PMPY | $8,385 | $7,469 | $6,764 | $7,607 | $8,834 | $7,407 |
| ED Visit Cost PMPY | $1,328 | $1,422 | $746 | $990 | $2,349 | $2,727 |
| Confirmed Violence Cost PMPY | $821 | $692 | $419 | $438 | $559 | $687 |
| Confirmed Violence Ann. Served Days | 1.6 | 1.2 | 0.8 | 0.9 | 1.1 | 0.8 |
| Post-Period | ||||||
| Total Cost of Care PMPY | $33,579 | $41,917 | $21,277 | $33,275 | $14,370 | $22,439 |
| Pharmacy Cost PMPY | $20,748 | $25,663 | $12,116 | $16,953 | $2,664 | $7,382 |
| Medical Cost PMPY | $12,831 | $16,255 | $9,161 | $16,322 | $11,706 | $15,056 |
| Admissions Cost PMPY | $4,764 | $6,242 | $3,612 | $9,739 | $4,766 | $6,728 |
| ED Visit Cost PMPY | $1,145 | $1,294 | $595 | $1,017 | $2,125 | $2,673 |
| Confirmed Violence Cost PMPY | $344 | $340 | $213 | $432 | $87 | $265 |
| Confirmed Violence Ann. Served Days | 0.9 | 0.7 | 0.6 | 0.8 | 0.2 | 0.3 |
| Table 3: Savings NET of Program Fees | ||||||
|---|---|---|---|---|---|---|
| Market 1 | Market 2 | Market 3 | ||||
| Total Cost of Care PMPY | $8,349 | 20% | $12,681 | 43% | $8,372 | 41% |
| Pharmacy Cost PMPY | $5,143 | 21% | $6,520 | 41% | $3,513 | 98% |
| Medical Cost PMPY | $3,208 | 18% | $6,161 | 46% | $4,859 | 29% |
| Medical Cost PMPY | $3,208 | 18% | $6,161 | 46% | $4,859 | 29% |
| Admissions Cost PMPY | $2,394 | 29% | $5,284 | 78% | $3,389 | 38% |
| ED Visit Cost PMPY | $55 | 4% | $178 | 24% | $170 | 7% |
| Confirmed Violence Cost PMPY | $125 | 15% | $200 | 47% | $48 | 9% |
| Confirmed Violence Ann. Served Days | 0.2 | 13% | 0.1 | 13% | 0.5 | 45% |
| Confirmed Violence Ann. Served Days | 2.8 | 4.3 | 2.8 | |||
| Table 4: Market 1 Subpopulation Return on Investment | ||||||
|---|---|---|---|---|---|---|
| Mindoula Members | Return Multiple | |||||
| Total Cost of Care PMPY | $8,349 | 20% | ||||
| Fibromyalgia, Chronic Pain, & Fatigue | 886 | 3.0 | ||||
| Diabetes | 597 | 3.3 | ||||
| MAT | 289 | 3.5 | ||||
| Heart Disease | 266 | 3.1 | ||||
| Liver Disease | 246 | 3.3 | ||||
| Stimulants | 235 | 4.8 | ||||
Conclusion
The results presented above suggest that US payors who choose to partner with Mindoula can play an important role in improving the health and wellbeing of populations impacted by interpersonal violence. They can do so in an economically sustainable way by adopting and implementing a market-leading data driven, tech-enabled program that delivers returns on investment which significantly exceed program fees. The success of Mindoula’s IVRP across 7 states is driven by Mindoula’s data science, program design and delivery, and staff training capabilities and delivers 2.8x to 4.3x returns on investment (ROI) net of fees. This performance provides sufficient evidence of program sustainability, and should encourage wider adoption. The evidence presented here should encourage health plans to increase their level of resource allocation so as to address the widespread and costly epidemic of violence that continues to plague our cities and towns, states, and regions, and the US as a whole.
Contributing authors: Glenda Wrenn Gordon, MD, MSHP; Kate Cordell, PhD, MPH, Jessica Sucik, LCSW; Melanie Bowen, JD; Justin Lanning; Blaise DeLuca, MHA; Brian Thomas
For further details, contact Justin Lanning, Chief Customer Officer, at justin.lanning@mindoula.com.
References
Mercy, J. A., Hillis, S. D., Butchart, A., Bellis, M. A., Ward, C. L., Fang, X., & Rosenberg, M. L. (2017). Interpersonal Violence: Global Impact and Paths to Prevention. In C. N. Mock (Eds.) et. al., Injury Prevention and Environmental Health. (3rd ed.). The International Bank for Reconstruction and Development / The World Bank.
Peterson, C., Kearns, M. C., McIntosh, W. L., Estefan, L. F., Nicolaidis, C., McCollister, K. E., Gordon, A., & Florence, C. (2018). Lifetime Economic Burden of Intimate Partner Violence Among U.S. Adults. American journal of preventive medicine, 55(4), 433–444. https://doi.org/10.1016/j.amepre.2018.04.049
Slutkin, G., Ransford, C., & Zvetina, D. (2018). How the Health Sector Can Reduce Violence by Treating It as a Contagion. AMA journal of ethics, 20(1), 47–55. https://doi.org/10.1001/journalofethics.2018.20.1.nlit1-1801
Tol W. A. (2020). Interpersonal violence and mental health: a social justice framework to advance research and practice. Global mental health (Cambridge, England), 7, e10. https://doi.org/10.1017/gmh.2020.4
Weitzman, A., & Goosby, B. J. (2020). Intimate partner violence, circulating glucose, and non-communicable Disease: Adding insult to injury?. SSM - population health, 13, 100701. https://doi.org/10.1016/j.ssmph.2020.100701
Thurston, R. C., Chang, Y., Matthews, K. A., Harlow, S., El Khoudary, S. R., Janssen, I., & Derby, C. (2022). Interpersonal Trauma and Risk of Incident Cardiovascular Disease Events Among Women. Journal of the American Heart Association, 11(7), e024724. https://doi.org/10.1161/JAHA.121.024724
Zhu, J., Exner-Cortens, D., Dobson, K., Wells, L., Noel, M., & Madigan, S. (2024). Adverse childhood experiences and intimate partner violence: A meta-analysis. Development and Psychopathology, 36(2), 929–943. https://doi.org/10.1017/S0954579423000196
Trabold, N., McMahon, J., Alsobrooks, S., Whitney, S., & Mittal, M. (2020). A Systematic Review of Intimate Partner Violence Interventions: State of the Field and Implications for Practitioners. Trauma, violence & abuse, 21(2), 311–325. https://doi.org/10.1177/1524838018767934
Albanesi, C., Tomasetto, C., & Guardabassi, V. (2021). Evaluating interventions with victims of intimate partner violence: a community psychology approach. BMC women's health, 21(1), 138. https://doi.org/10.1186/s12905-021-01268-7
Blasdell R. (2021). The co-occurrence of physical and sexual intimate partner violence among US college females. International Journal of Criminal Justice Sciences, 169(1), 97–109.
Chiaramonte, D., Schick, M. R., Woerner, J., Hernandez, A. J., & Sullivan, T. P. (2024). Elucidating Heterogeneity of Intimate Partner Violence Among Women: Latent Class Analysis of Daily IPV, PTSD, and Substance Use Collected via Experience Sampling Methodologies. Journal of Interpersonal Violence, 0(0). https://doi.org/10.1177/08862605241286026
Miller, C. J., Adjognon, O. L., Brady, J. E., Dichter, M. E., & Iverson, K. M. (2021). Screening for intimate partner violence in healthcare settings: An implementation-oriented systematic review. Implementation research and practice, 2, 26334895211039894. https://doi.org/10.1177/26334895211039894
Sheppard, L., Alsubhi, M., Brown, V., Le, H., Robinson, K., & Moodie, M. (2024). What Interventions are Cost Effective in Reducing Violence Against Women? A Scoping Review. Applied health economics and health policy, 22(3), 283–296. https://doi.org/10.1007/s40258-023-00870-0
Billioux, A., Verlander, K., Anthony, S., & Alley, D. (2017). Standardized screening for health-related social needs in clinical settings: the accountable health communities screening tool. NAM perspectives.
Gaynes, B. N., DeVeaugh-Geiss, J., Weir, S., Gu, H., MacPherson, C., Schulberg, H. C., Culpepper, L., & Rubinow, D. R. (2010). Feasibility and diagnostic validity of the M-3 checklist: a brief, self-rated screen for depressive, bipolar, anxiety, and post-traumatic stress disorders in primary care. Annals of family medicine, 8(2), 160–169. https://doi.org/10.1370/afm.1092
Centers for Medicare & Medicaid Services. Chronic Conditions Algorithms. Chronic Conditions Data Warehouse. Published 2022. Accessed October 29, 2024. https://www2.ccwdata.org/documents/10280/19139421/chr-chronic-condition-algorithms.pdf
Webster, D. W., Richardson, J., Meyerson, N., Vil, C., & Topazian, R. (2022). Research on the Effects of Hospital-Based Violence Intervention Programs: Observations and Recommendations. The ANNALS of the American Academy of Political and Social Science, 704(1), 137-157. https://doi.org/10.1177/00027162231173323
Peterson, C., & Kearns, M. C. (2021). Systematic review of violence prevention economic evaluations, 2000–2019. American journal of preventive medicine, 60(4), 552-562.
O'Toole, M. J., Schnippel, K., & Larson, B. (2023). Hospital-based violence intervention programs: An analysis of costs and key components. Journal of Trauma and Acute Care Surgery, 10-1097.
Basile, K.C., Smith, S.G., Kresnow, M., Khatiwada S., & Leemis, R.W. (2022). The National Intimate Partner and Sexual Violence Survey: 2016/2017 Report on Sexual Violence. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention.
Fazel, S., Burghart, M., Wolf, A., Whiting, D., & Yu, R. (2024). Effectiveness of Violence Prevention Interventions: Umbrella Review of Research in the General Population. Trauma, violence & abuse, 25(2), 1709–1718. https://doi.org/10.1177/15248380231195880